Everything you ever wondered about vaccines
From internationally renowned medical discussion to neighborhood small talk, vaccines have been at the forefront of conversation over the past few months. They’ve served as a welcome distraction from the monotony of pandemic life, and as a much needed spark of hope!
Some are excited, some apprehensive, and everyone seems to have something to say. But how much do we all really understand about how immunization works? When I asked myself that question I realized the answer pretty quickly: not enough. So I set out to change that. And when I finished, I thought you all might be curious too.
Immunization essentials
The ancient history of vaccines
The practice of inoculation has existed for over a thousand years. The first confirmed instances of its use have been traced to China and India in the 1500s, though some suggest it came about as early as 200 BCE.
Inoculation was a messy business back then – achieved through a method called variolation. This involved inhaling crushed up smallpox scabs or by rubbing matter from smallpox sores into small cuts in the skin. Usually variolized patients contracted a milder version of the deadly disease, but results were unpredictable and the process was inconvenient.
According to History.com: “Variolization… had a case fatality rate of 5 to 10 percent. And even if all went well, inoculated patients still needed a month to recover. The procedure was not only risky for the individual patient, but for the surrounding population. An inoculant with a mild case might feel well enough to walk around town, infecting countless others with potentially more serious infections.”
This ancient immunization technique was only developed against smallpox, which was ubiquitous and deadly. It eventually made its way to the Western world and was employed up until the invention of the modern vaccine about 200 years ago. Fascinatingly, variolation was introduced to New England by a man named Onesimus, who was enslaved to Cotton Mathers (of the Salem Witch Trials). Though he likely never knew, Onesimus saved hundreds of lives, and might have even helped establish our country! Many historians credit George Washington’s insistence that his troops undergo variolation as a crucial part of American victory during the Revolutionary War.
In 1796, long after the invention of variolation, a British physician named Edward Jenner made the next great breakthrough in public health science. He inoculated a young boy with cowpox pustules instead of smallpox after observing that humans have a less severe reaction to the bovine disease. The boy had none of the severe symptoms of the smallpox inoculation, but did show immunity to smallpox. Thus, the first modern vaccine was born.
Vaccination is set apart from variolation because it employs innocuous versions of a disease agent. This makes it far less fatal. Over the next few centuries, “scientists following Jenner’s model developed new vaccines to fight numerous deadly diseases, including polio, whooping cough, measles, tetanus, yellow fever, typhus, and hepatitis B.”
How do vaccines work?
Vaccines work by initiating the body’s natural immune response. They simulate bacteria and viruses without inducing symptoms of illness, giving the body a chance to develop defense mechanisms in preparation for a legitimate attack. For context, the body’s natural defense mechanisms consist of three types of white blood cells:
1. Macrophages
These specialized cells are on perpetual cellular clean up duty. They target bacterial or viral invaders, dead cells, and other harmful organic items. They then “swallow them” in a process called phagocytosis, digest them, and respond by presenting antigens. What’s an antigen? It’s “a molecule or molecular structure, such as may be present on the outside of a pathogen, that can be bound by an antigen-specific antibody or B-cell antigen receptor.” In other words, it’s a danger signal to the body that stimulates an immune response.
2. B-lymphocytes
B-lymphocytes play molecular defense. These white blood cells “recognize soluble antigens via immunoglobulins anchored on their surface and differentiate into antibody-producing cells.” Put simply, they make antibodies which attack antigens left behind by macrophages.
Antibodies are “specialized, Y-shaped proteins that bind like a lock-and-key to the body’s foreign invaders.” Sometimes they are referred to as immunoglobulins.
3. T-lymphocytes
T-lymphocytes are also bodily defenders. Their job is to take out cells that have already been infected by pathogens. T-lymphocytes are also called memory cells, because they “remember” the effective immune response when the body encounters the same antigen multiple times. They’re the reason you can’t get chicken pox twice.
Thus, vaccines work because they cause the body to make protective antibodies and memory cells BEFORE it encounters a real pathogen.
What are the different types of vaccines?
The CDC and the HHS (Department of Health and Human Services) provide very accessible summaries of the way that each traditional type of vaccination works. They lay it out better than I could, so I’ve pulled several explanations directly from their public resources. This list is not extensive, but it includes the major vaccine types. Use the links above for the original source pages and more information.
- Live, attenuated vaccines fight viruses and bacteria. These vaccines contain a version of the living virus or bacteria that has been weakened so that it does not cause serious disease in people with healthy immune systems. Because live, attenuated vaccines are the closest thing to a natural infection, they are good teachers for the immune system. Examples of live, attenuated vaccines include measles, mumps, and rubella vaccine (MMR) and varicella (chickenpox) vaccine. Even though they are very effective, not everyone can receive these vaccines. Children with weakened immune systems—for example, those who are undergoing chemotherapy—cannot get live vaccines.
- Inactivated vaccines also fight viruses and bacteria. These vaccines are made by inactivating, or killing, the germ during the process of making the vaccine. The inactivated polio vaccine is an example of this type of vaccine. Inactivated vaccines produce immune responses in different ways than live, attenuated vaccines. Often, multiple doses are necessary to build up and/or maintain immunity.
- Toxoid vaccines prevent diseases caused by bacteria that produce toxins (poisons) in the body. In the process of making these vaccines, the toxins are weakened so they cannot cause illness. Weakened toxins are called toxoids. When the immune system receives a vaccine containing a toxoid, it learns how to fight off the natural toxin. The DTaP vaccine contains diphtheria and tetanus toxoids.
- Subunit, recombinant, polysaccharide, and conjugate vaccines use specific pieces of the germ—like its protein, sugar, or capsid (a casing around the germ). Because these vaccines use only specific pieces of the germ, they give a very strong immune response that’s targeted to key parts of the germ. They can also be used on almost everyone who needs them, including people with weakened immune systems and long-term health problems.One limitation of these vaccines is that you may need booster shots to get ongoing protection against diseases.
- Viral vector vaccines involve a modified version of a virus which is NOT the pathogen the vaccine protects against. Called the vector, this modified virus uses cells to make a spike protein (which is unique to the coronavirus). The body identifies the spike protein as a threat and begins producing antibodies. Several different viruses have been used as vectors, including influenza, vesicular stomatitis virus (VSV), measles virus, and adenovirus, which causes the common cold. Adenovirus is one of the viral vectors used in some COVID-19 vaccines being studied in clinical trials. Johnson and Johnson and AstraZeneca are both viral vector vaccines.
- mRNA vaccines send the body instructions to manufacture a specific protein – the part of COVID-19 that the body recognizes as a threat. When cells display this protein the body begins producing antibodies, effectively building an immune response to the actual virus. The mRNA doesn’t persist in the cells after the protein is produced.
Though mRNA vaccines were not available to the public until recently, their development has been a decades-long process. And they are not the only DNA based vaccination technology being studied. According to the CDC, “Interest has grown in these vaccines because they can be developed in a laboratory using readily available materials. This means the process can be standardized and scaled up, making vaccine development faster than traditional methods of making vaccines.” Pfizer and Moderna are both mRNA vaccines.
What’s in them?
Vaccine ingredients do three things: provide immunity, extend the life of the vaccine, and play a role during production. They are almost always things we are exposed to in our normal activities. For example, sugar and gelatin, two vaccine stabilizers, are found in Jell-O. If you want more information, check out this link.
Conspiracies debunked
Vaccines have unwavering support within the scientific and medical communities. Anti-vaccination sentiment has existed from the time of their invention, but for the vast majority of people no adverse long term health side effects have been attributed to vaccine administration. The connection between vaccines and autism – maybe the most famous concern – has long since been discarded. If you’re looking for more information on this topic, Vox has a thorough explainer to direct your research.
Conquering coronavirus
Where were the COVID-19 vaccines developed and who developed them?
The Pfizer vaccine was developed in a partnership between two companies, Pfizer and BioNTech. Pfizer is based in New York City while BioNTech is based in Mainz Germany. The actual formula was developed by BioNTech founders Ugur Sahin and Ozlem Tureci. You can meet that groundbreaking duo here.
The Moderna vaccine came from even closer to home – the company is based in Cambridge, MA! It was developed in partnership with the National Institute of Allergy and Infectious Disease. Work began last January, and they provide a handy timeline of their progress.
Johnson and Johnson is another American-based company, with headquarters in New Brunswick, NJ. This decades old pharmaceutical giant worked with its own Janssen Pharmaceutical Companies as well as with the Biomedical Advanced Research Authority and Beth Israel Deaconess Medical Center. The Johnson and Johnson vaccine distribution has been paused due to concern over a potential connection to blood clots.
Have these vaccines been thoroughly vetted?
Vaccine development occurs in 6 stages:
- Exploratory stage
Scientists study the pathogen and design candidate vaccines. They run lab tests until they discover a formula that holds the significant promise.
- Pre-clinical stage
More rigorous testing moves forward with the selected candidate. Clinical development requires human participants, so in this stage all measures are taken to understand and predict how the vaccine will function in humans. Animal testing is employed.
- Clinical development
Clinical development occurs in 3 phases. According to the CDC: “During Phase I, small groups of people receive the trial vaccine. In Phase II, the clinical study is expanded and vaccines are given to people who have characteristics (such as age and physical health) similar to those for whom the new vaccine is intended. In Phase III, the vaccine is given to thousands of people and tested for efficacy and safety.”
Before drug companies are allowed to begin clinical testing the FDA performs a thorough check of the vaccine candidate and the laboratory process used to make it.
“FDA evaluation includes an assessment of the preclinical data and a determination whether these tests were conducted according to Good Laboratory Practices,” a statement from the FDA website reads.
- Regulatory review and approval
After clinical trials, new vaccinations have to go through a very thorough review process at the FDA before being administered to the general public. According to the FDA, Product License applications include the following:
- a detailed description of the manufacturing procedures, testing methods, and process controls for the product
- results of all laboratory tests performed on a specified number of lots (including stability testing)
- results of clinical studies
- proposed labeling
Manufacturers must also apply for an Establishment License, which requires them to submit information on their manufacturing facilities, equipment, production practices, employees, and more.
- Manufacturing
Once a vaccine has been approved, it goes into production. Manufacture is closely monitored. In fact, the FDA requires vaccine manufacturers to submit data to support manufacturing processes, facilities, product characterization, and demonstration of lot-to-lot consistency.”
- Quality control
To put it simply, they just keep on observing the way the vaccine affects people. For years.
Vaccine development generally takes between 10-15 years, but that does not mean that companies like Pfizer or Moderna were allowed to cut corners. Rather, previous knowledge of the nature of coronaviruses, global collaboration, and increased funding from the public and private sector expedited the process. In other words, those 5-10 years can be reduced significantly when companies aren’t strapped for cash and are able to share resources. The FDA is also aware that special circumstances require special protocol, and have rules in place to expedite vaccine development without putting the public at risk.
From the FDA: “In public health emergencies, such as a pandemic, the development process may be atypical or expedited. For example, as demonstrated by the response to the COVID-19 pandemic, the U.S. government may coalesce government agencies, international counterparts, academia, nonprofit organizations and pharmaceutical companies to develop a coordinated strategy for prioritizing and speeding development of the most promising treatments and vaccines.”
Which COVID-19 vaccine is the most effective?
All three are highly effective. Each has been successful in preventing deaths and hospitalizations.
And even though Moderna and Pfizer showed a higher efficacy rate than Johnson and Johnson in clinical trials, we can’t jump to the conclusion that it’s less effective. There are lots of variables that make comparing efficacy rates misleading. Clinical trials for each vaccine were held at different times and carried out in different ways. For example, the infection rate at the time of clinical trials and the healthcare available to participants both have the potential to change the outcome.
What are the side effects? What does it mean if I have them (or if I don’t)?
Some people have minor reactions when they get vaccinated, some have pronounced reactions, and some have no reaction at all. This has nothing to do with how effectively the vaccination provided immunity.
Is there a chance of me getting severe side effects many years in the future?
There is pretty much no chance of anybody getting severe side effects in the future. In an interview for Vox, Microbiology professor Deborah Fuller explained: “The idea that they’re [vaccines] going to cause some sort of issue five, 10 years from now, that just doesn’t happen. That’s just not how vaccines work, they get in, they do their job, they go away. The only thing a vaccine does is stimulate an immune response.”
Special situations: is it safe for breastfeeding, or immunocompromised people to get vaccinated?
In both of these cases the answer is yes. There is no evidence of people with autoimmune disorders getting adverse side effects from the COVID-19 vaccine. And mothers naturally transfer immunity to all sorts of pathogens to their babies when they nurse.
How will vaccine science evolve with COVID-19 and its variants?
COVID vaccine science is evolving quickly and there are some really cool new technologies on the horizon.
“Researchers are racing to develop the next generation of COVID-19 vaccines, utilizing a variety of innovative technologies to produce more convenient and more potent options,” said an article from NPR, “Some of the new vaccines are already being tested in volunteers and could even be available for distribution in the next year or so.”
This means vaccines that come in the form of tablets or nasal spray, and could be self administered. Additionally, new means of transferring the actual immunity are being explored. Modifying the spike protein – which initiates the immune response – could lead to the development of a more potent vaccine formula. The fight against COVID-19 far from over. Scientists and doctors are continuing to work to make vaccinations accessible and convenient, as well as safe and effective.

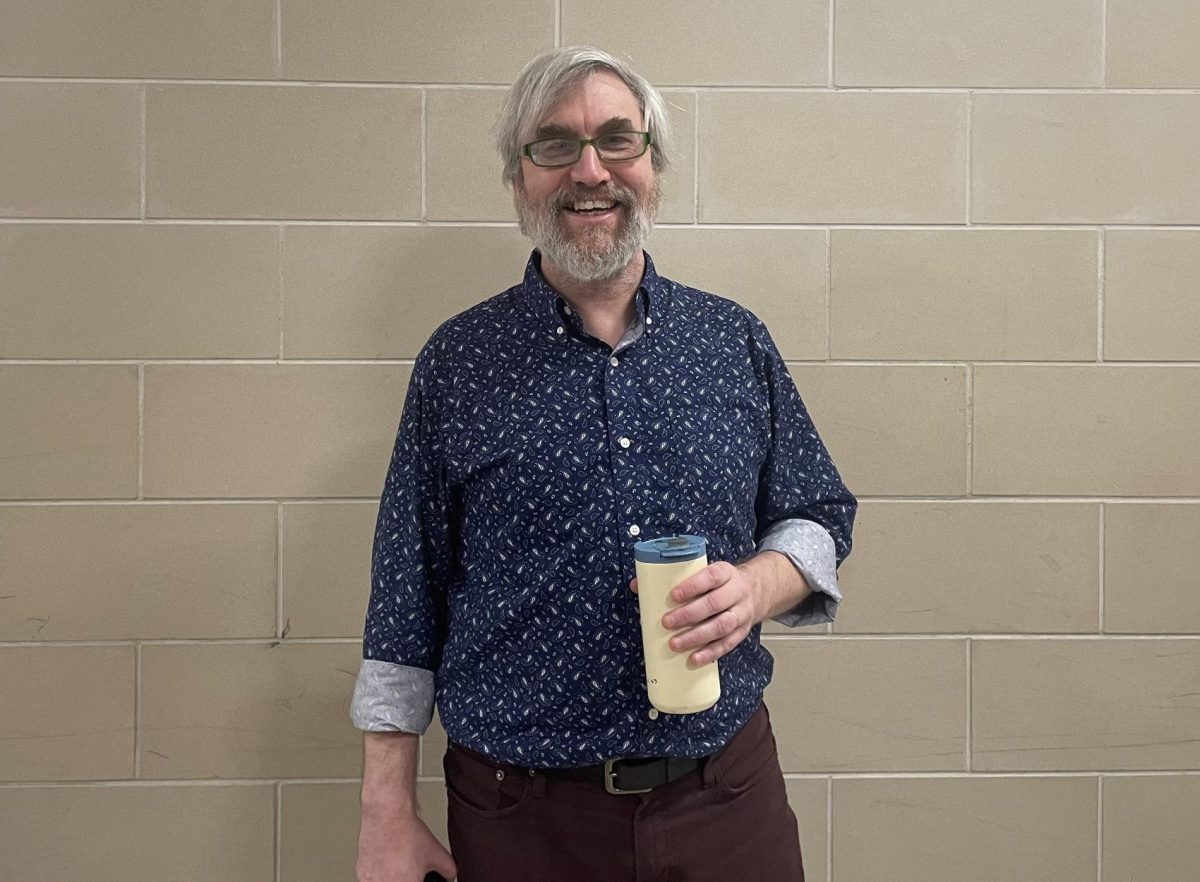
Mila Barry is in her fourth year at Gloucester High School, and her third year on the Gillnetter staff. Outside of writing for the newspaper, she’s...